Auth Workflows
An authorization workflow tracks the process of obtaining an authorization (or re-authorization) for services through submission, review, and approval of an assessment report.
There are 3 workflow types:
- New Auth - for new patients receiving an initial assessment.
- Re-auth - for existing patients received a follow-up assessment for reauthorization of services.
- Continuity of Care - for existing patients who do not need a new follow-up assessment, but do need a new authorization request (e.g., for switching organizations mid-authorization).
The workflow type can be viewed or set in the header of the authorization workflow.
Auth Workflow Creation
An authorization workflow can be created the following ways:
- Manually- Select 'Auth Workflows' on the site menu in the CRM Area to open the Auth Workflow Main Grid. Click 'New' to create a new auth workflow.
- Automatically-
- A 'New Auth' auth workflow is automatically created when a new patient opportunity is created. The opportunity field will be automatically populated on the auth workflow.
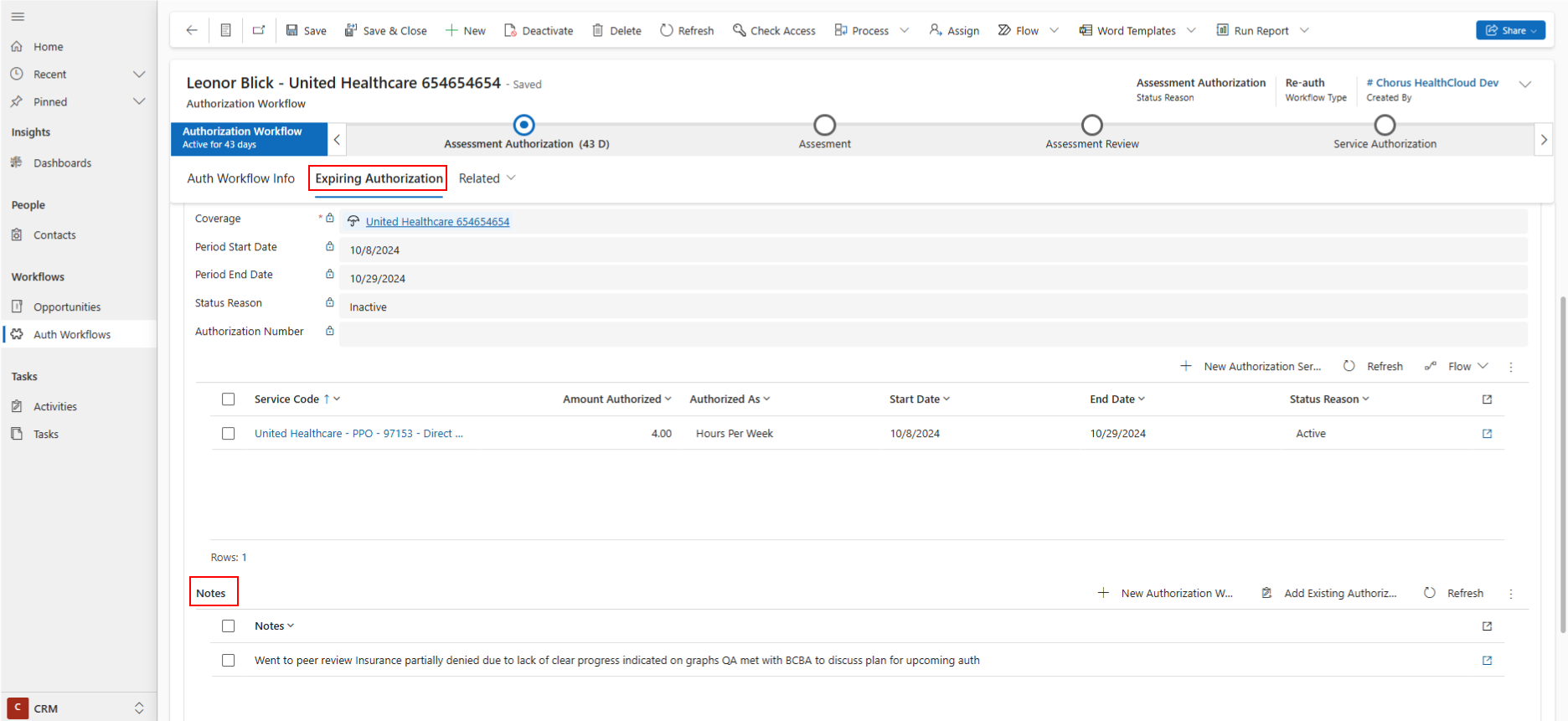
- A 'Re-auth' auth workflow is automatically created a certain number of weeks before a service authorization expires. The number of weeks is set on the business unit of the authorization. The expiring authorization will be automatically populated on the auth workflow.
The expiring authorization details and services can be viewed on the Expiring Authorization tab. Notes from the previous authorization workflow can also be viewed there. Learn more about authorizations.
Auth Workflow Stages
Authorization workflows have 4 stages:
- Assessment Authorization
- Assessment
- Assessment Review
- Service Authorization
Assessment Authorization
The Assessment Authorization stage is about obtaining an authorization for initial/follow-up assessment service.
- Request Submitted - enter the date the request for the assessment authorization was submitted.
- Assessment Authorization Status - enter the status of the authorization request (approved/denied).
- Assessment Authorization - once the authorization was received, click 'New Authorization' in the Assessment Authorization field to create the assessment authorization.
When an assessment authorization is received, click 'Next Stage' to move the authorization workflow to the Assessment stage.
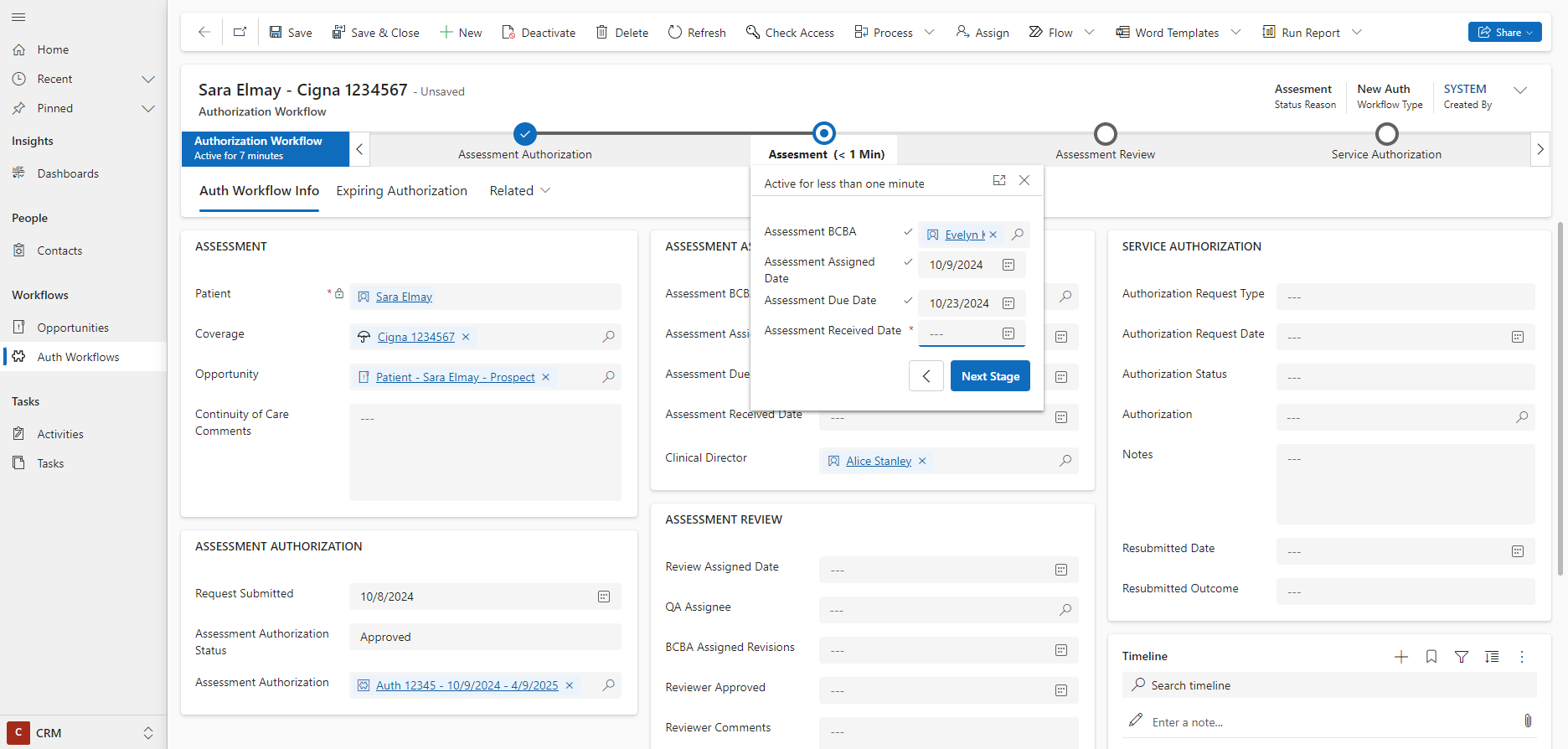
Assessment
The Assessment stage is for assigning a BCBA to write an assessment report, and tracking it is received in a timely fashion.
- Assessment Assignment - choose an assessment care team assignment from the assessment/expiring authorization, or create a new one by clicking '+ New'.
- Assessment BCBA - the Assessment BCBA will be populated based on the Assessment Assignment.
- Assessment Assigned Date - enter the date the BCBA was assigned to write the report. This will auto-populate with today's date when the assessment BCBA is populated.
- Assessment Due Date - enter the due date the BCBA was given for submitting the completed report. This will auto-populate with today's date plus the number of weeks populated on the business unit of the authorization.
- Assessment Received Date - enter the date the BCBA submitted the completed report.
When an assessment report is received, click 'Next Stage' to move the authorization workflow to the Assessment Review stage.
Assessment Review
The Assessment Review stage is for assigning QA personnel to review the assessment report, request revisions, and approve the report.
- Review Assigned Date - enter the date the QA reviewer was assigned to review the assessment report.
- QA Assignee - select the QA reviewer who is assigned to review the report. Only practitioners with a current BCBA practitioner role will show as options here.
- BCBA Assigned Revisions - enter the date the QA assignee requested revisions from the BCBA who wrote the report.
- Reviewer Approved - enter the date the QA assignee reviewed the report/revisions.
- Reviewer Comments - enter any comments the QA assignee has regarding the report.
When an assessment report is approved by a QA reviewer, click 'Next Stage' to move the authorization workflow to the Service Authorization stage.
Service Authorization
The Service Authorization stage is for requesting an authorization from the payer, and creating the authorization once received.
- Authorization Request Type - select the mode through which an authorization was requested from the payer (payer portal / email / phone / fax).
- Authorization Request Date - enter the date the authorization was requested.
- Authorization Status - enter the payer response to the authorization request (approved / partially denied / denied).
- Authorization - click 'New Authorization' in the Authorization field to create the authorization received by the payer, or open the expiring authorization and click Clone Authorization to create a copy of the past authorization and update its details. Learn more about authorizations.
- Notes - enter any notes about the approval/denial, insurance feedback, or peer review comments.
- Resubmitted Date - enter the date the authorization request was resubmitted to the payer (if relevant).
- Resubmitted Outcome - enter the payer response to the resubmitted authorization request (approved / partially denied / denied).
When the service authorization was approved and entered onto the authorization workflow, click Finish to set the status reason to Completed and deactivate the workflow. At this point, the opportunity is completed, and the patient's episode of care will automatically move from Planned to Active to show they have completed intake and are ready for services.
Auth Workflow Emails
New auth and Re-auth authorization workflows generate a draft email to the assessment BCBA with patient and past authorization information to streamline communication and provide the details the BCBA needs to write a report.
- On the Assessment stage of the auth workflow, select the Assessment BCBA. The assigned date will auto-populate with today's date, and the assessment due date will auto-populate with today's date plus the number of weeks populated on the business unit of the patient. You can adjust these dates if needed.
- Click 'Save'.
- Refresh the page. A draft email will appear on the auth workflow timeline.
The email template can be customized to your organization's needs. Speak to your account manager about customizing the messaging in the email.
- The Initial Assessment Email includes relevant patient information to help the BCBA complete an initial assessment report. It also specifies the due date of the report.
- The Reassessment Email includes relevant patient information to help the BCBA complete a reassessment report. The details of the previous authorization services are listed in the email. It also specifies the due date of the report.
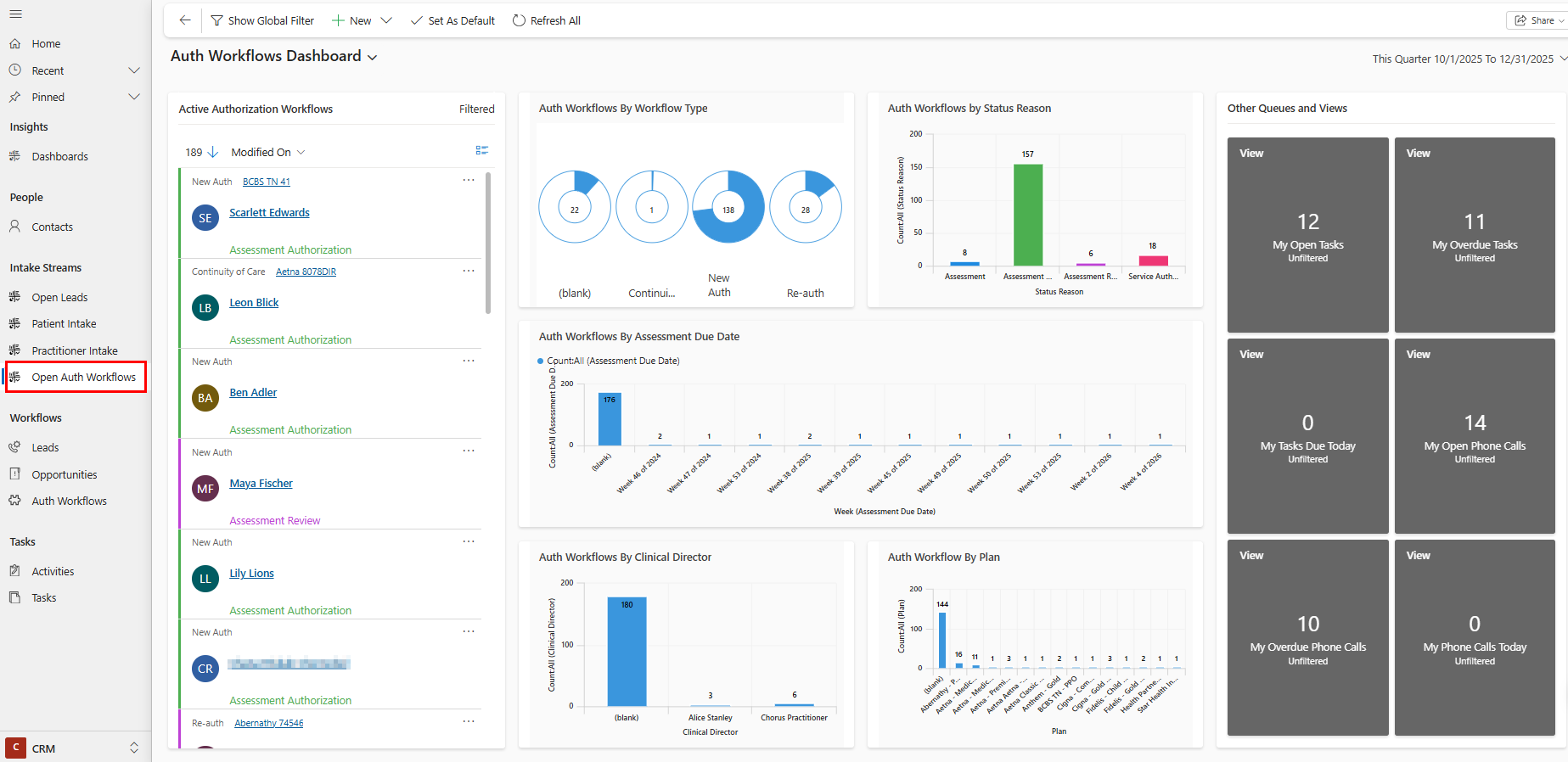
Auth Workflow Dashboard
Go to 'Dashboards' on the site menu and select the Authorization Workflow Dashboard to review:
- Assessments to assign (no assessment BCBA populated on auth workflow yet)
- Assessments in progress (auth workflows at the assessment stage, with the assigned date populated and received date blank)
- Overdue assessments (auth workflows at the assessment stage, with the assigned date populated and received date blank, and past the due date)
- Assessments to review (auth workflows at the assessment review stage where revisions were not assigned yet)
- Assessments awaiting revisions (auth workflows at the assessment review stage where revisions were assigned and reviewer did not approve yet)
- Authorizations to request (auth workflows where either the initial or service auth request date is blank)
- Open authorization requests (auth workflows where either the initial or service auth is blank)
- Resubmitted authorization requests (auth workflows where the resubmitted date is populated and the authorization is blank)
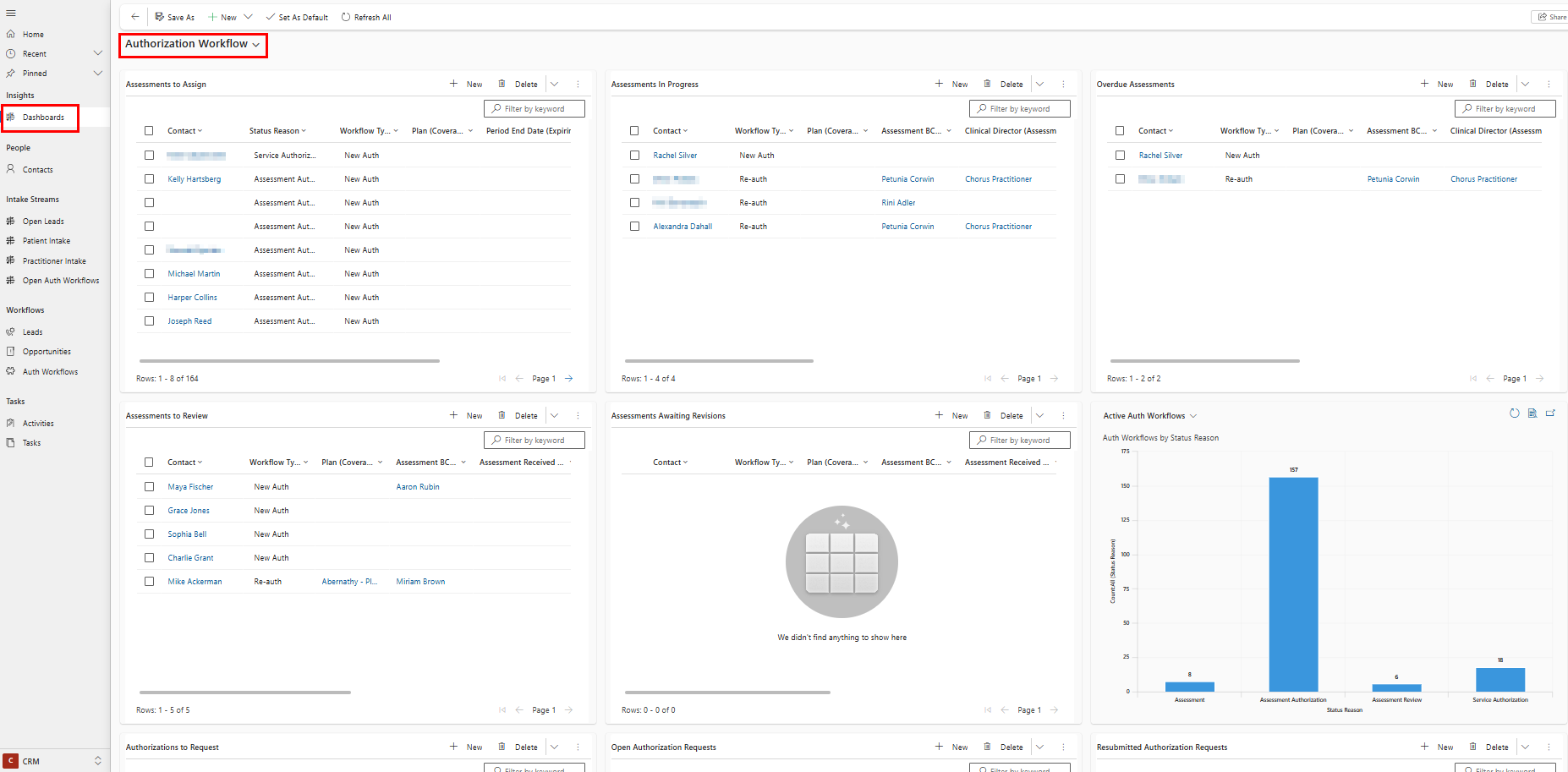
Open Auth Workflows Stream
Use the Open Auth Workflows Stream to efficiently work through open authorization workflows opportunities. Filter by any visual(s) on the dashboard to filter your stream and allow you to take next steps on open records easily:
- Workflow Type
- Auth workflow status reason
- Week of assessment due date
- Assessment BCBA's clinical director
- Patient's insurance plan
You can also jump to your open tasks or phone calls from the tiles on the right side of the dashboard.